Member Forms
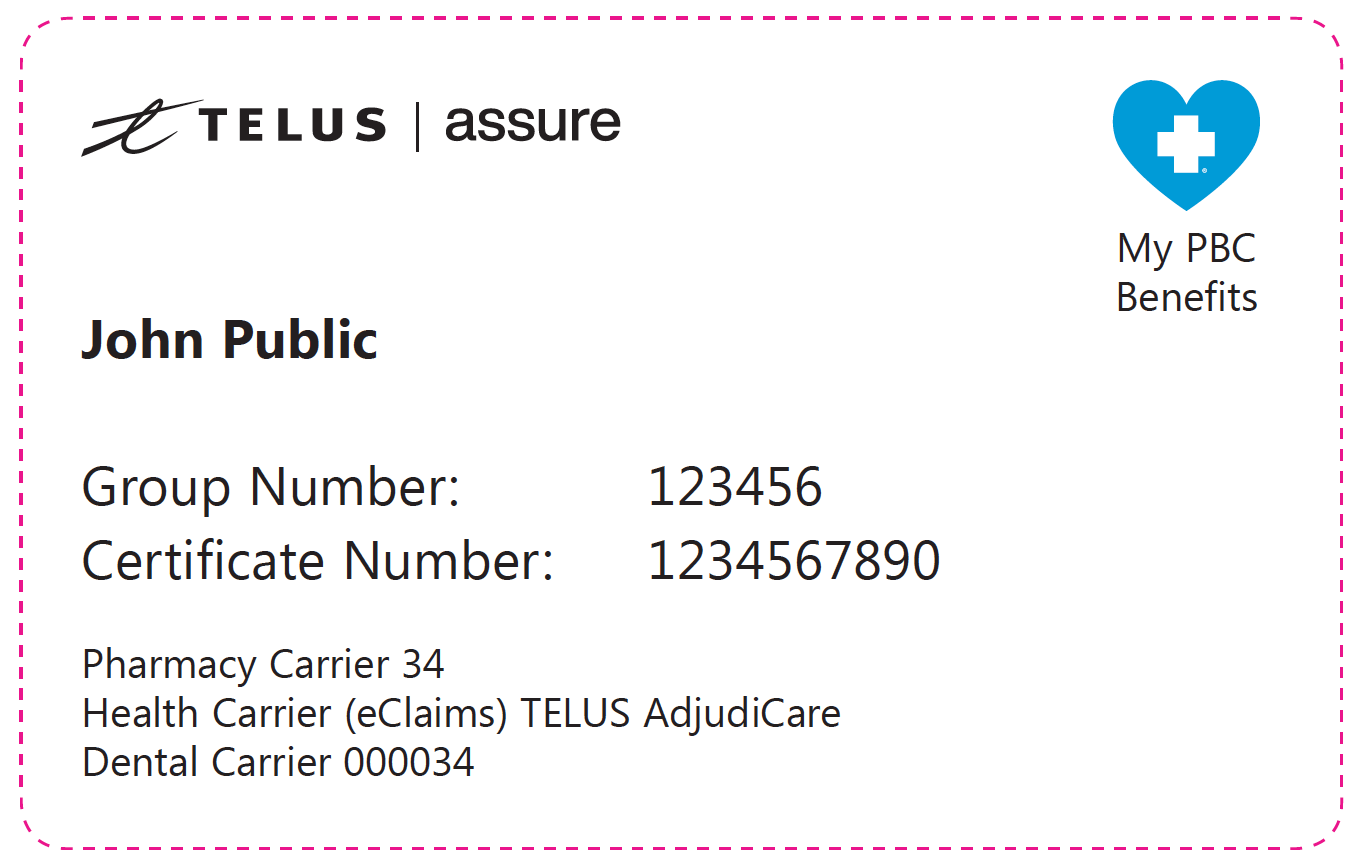 Sample Member ID card for My PBC Benefits" width="" />
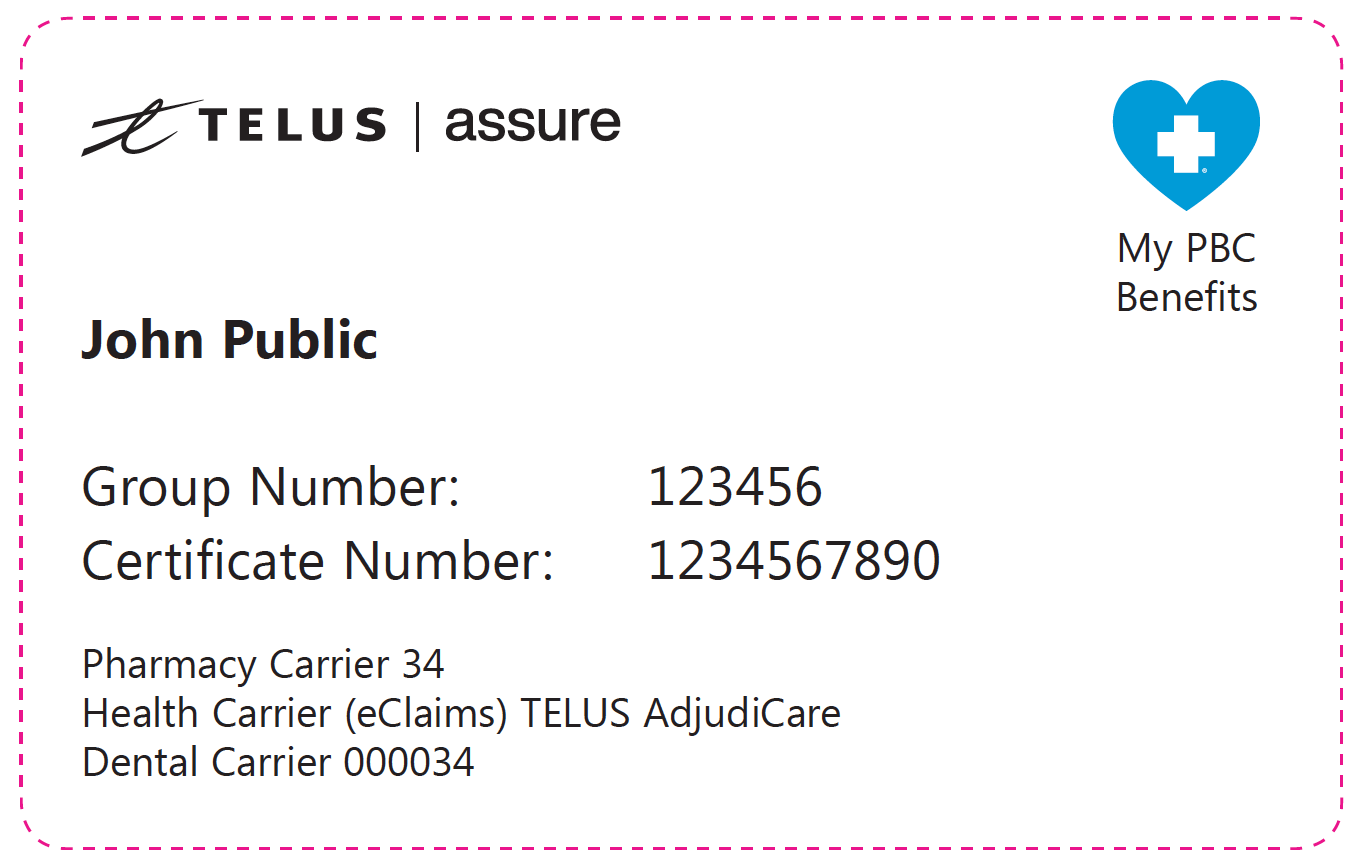
Sample Member ID card for My PBC Benefits" width="" />
If your membership card looks like this, please go to the My PBC Benefits resource page:
National Extended Health Care Claim Form [FORM-210 English] Use this form to submit claims for any health expenses covered under the provisions of your benefit plan.
National Claim Form (All benefit lines) [FORM-363 English]
National Claim Form - Health Spending Account [FORM-376 English]
-->
For Veteran Affairs, Canadian Forces and RCMP members
- Health care providers looking for claim forms for Veterans Affairs Canada (VAC), Royal Canadian Mounted Police (RCMP) or Canadian Forces (CF) members can contact our Federal Administered Programs Department by calling 1-888-261-4033 toll free.
- RCMP members — must submit a 1393 form available through your detachment. Your completed 1393 form should be sent to:
RCMP Health Services
Mailstop #1208
14200 Green Timbers Way
Surrey, BC
V3T 6P3
For Travel Claims and Out-of-Country/Province claims
- Out-of-Country and Out-of-Province Coverage and Claims — Click here to obtain claim forms and instructions for claiming emergency medical expenses.
- Trip Cancellation / Baggage Claim Form - Use this form to claim for Trip Cancellations or Lost Baggages.
- Visitors to Canada Travel Plan Claim Form - Use this form if you are claiming against a Visitors to Canada Travel Plan contract
- Travel Premium Refund Request Form
For Ministry of Social Development & Poverty Reduction or Health Kids Clients
Miscellaneous forms
- Blue Chip Drug Eligibility Inquiry Form — Blue Chip plans require prior authorization on certain drugs before we can reimburse prescription costs.
- Individual Plan Pre-Authorized Debit Form — Use this form to provide Pacific Blue Cross with pre-authorization to debit your individual plan premiums from your financial institution.
- Direct Deposit Registration — Sign-in to Member Profile to register for direct deposit, and receive electronic claim statements.
- Request for Claims History — Use this form to request a history of your health or dental claims for up to 5 years or more. NOTE: You can access up to 24 months of claim history for free in Member Profile.
- Accident or Injury Reimbursement Agreement — Complete this form if your health, dental or disability claim is the result of an accident or injury not related to a workplace or automobile incident.
- Accident or Injury Reimbursement Agreement (ICBC) — Health, dental or disability claim for a VEHICULAR accident or injury prior to November 9, 2018 .
- Accident or Injury Reimbursement Agreement (WorkSafe) — Health, dental or disability claim for a WORKPLACE accident or injury.
- Prior Authorization for High Cost Drugs — Certain new high cost drugs require prior authorization before we can reimburse prescription costs.
- Sleep Apnea Device Pre-Determination Form — Use this form to request a pre-determination on whether your sleep apnea device will be covered under your benefit plan.
- Member Assignment of Payment Form — When this form is completed and received by Pacific Blue Cross, it allows us to pay a person or party other than the plan holder. All original receipts and invoices must be attached.
- Blue Cross Life Insurance forms from Assumption Life
Additional Blood Glucose Test Strips
Please have your Endocrinologist or Diabetes Specialist complete this form to request an additional 100 blood glucose test strips, if circumstances warrant a periodic increase in blood glucose testing beyond your annual limit.
Glucose Monitoring Systems
If this request is for the Dexcom G6/G7 Continuous Glucose Monitor or the FreeStyle Libre 2 Flash Glucose Monitoring System (Libre 2), please have your Prescriber or Diabetes Specialist complete the BC PharmaCare Special Authority form and apply directly to BC PharmaCare on your behalf.
For members residing outside of BC, please have your Prescriber or Diabetes Specialist complete the Dexcom G6/G7/FreeStyle Libre 2 (Libre 2) request form.
- CGM INITIAL Request Form — If this is your first time request.
- CGM RENEWAL Request Form — To renew your request after 1 year and subsequent years.
*Electronic claims service is available to all Individual Plan customers and to group plan members whose plan sponsors/employers have opted to provide this service as part of their benefits plan
.

 Sample Member ID card for My PBC Benefits" width="" />
Sample Member ID card for My PBC Benefits" width="" />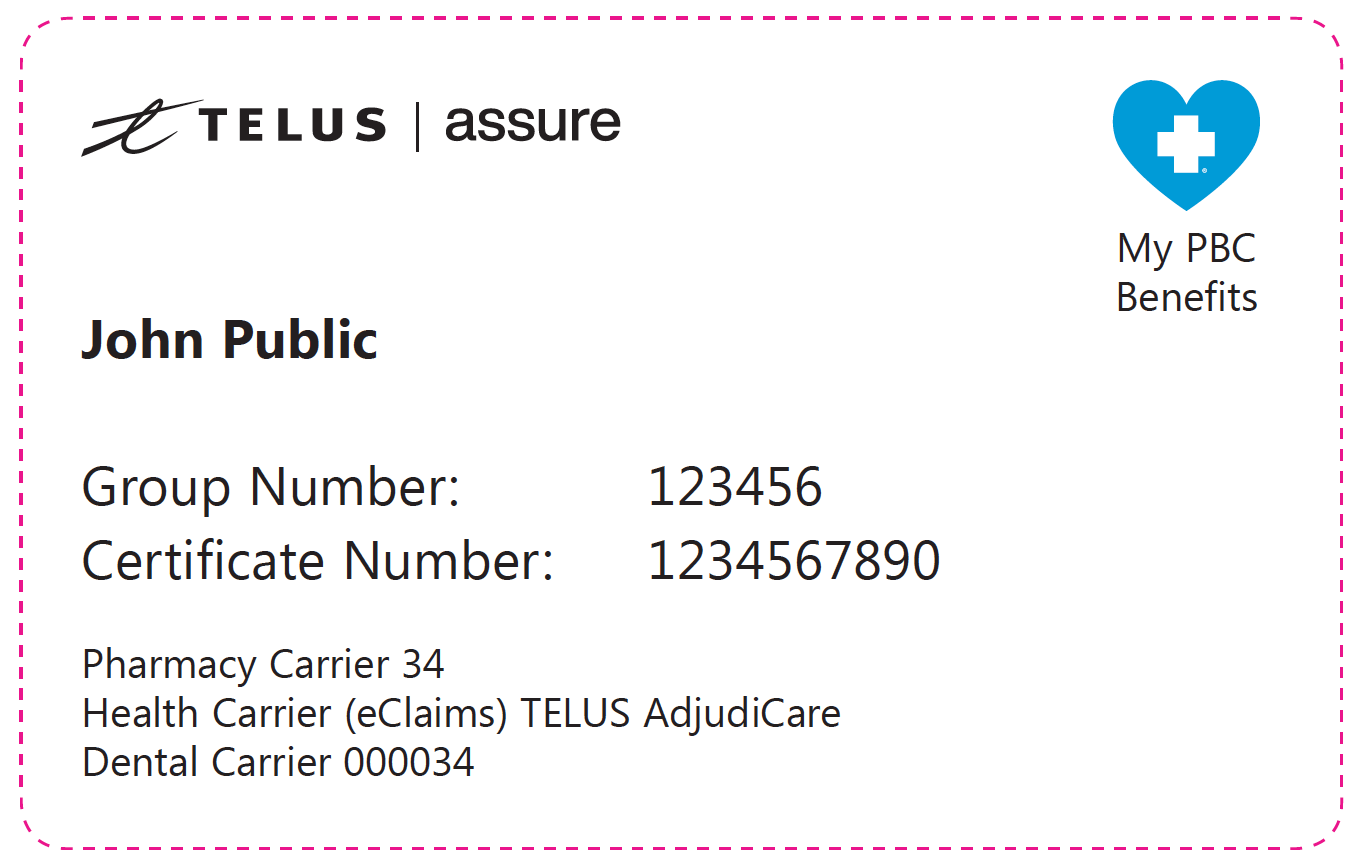 Sample Member ID card for My PBC Benefits" width="" />
Sample Member ID card for My PBC Benefits" width="" />